Cost Containment for Hospitals: Responding to the Rising Costs of Healthcare
March 22, 2022
What Is Hospital Cost Containment?
Cost containment in healthcare has always been a top concern for hospitals, especially in recent years due to unexpected events and changes in the market. Before jumping into the hospital cost containment strategies that healthcare leaders have used to weather these storms, we need to understand what hospital cost containment truly is.
Cost containment can be difficult to define, causing further problems when trying to reduce healthcare expenses. When hospital leaders discuss costs, some refer to price, while others refer to charges or reimbursement. The first step to designing an effective cost containment strategy is to understand a common definition of the term.
Hospitals design, implement and follow cost containment strategies to continuously reduce the cost of care while providing high quality care to customers. Cost containment strategies are typically long-term goals that directly impact the hospital’s finances. To effectively create cost containment strategies, effective communication needs to be occurring across all departments in hospitals
In an interview in Becker’s Hospital CFO Report, leaders at Eisenhower Medical Center shared their perspective on how important it is for physicians to understand cost data to effectively follow through with cost containment strategies.
Scott Gearing, Vice President of Surgical Services, and Ken Wheat, Senior Vice President and CFO, shared the following:
“You’ve got to be able to translate the data. You must be able to deliver the insights to clinicians in real time… Invest heavily in your data systems and put the right people around the table, and make sure some of those people are physicians. They have the power to either improve efficiency or drive-up costs. You really have to get the physicians around the table.”
Why should we care about cost containment? Sources including the American Medical Association have long shared the concern in the rising costs of healthcare. As healthcare leaders, it is important to understand what is driving these high costs to create effective strategies to contain them. In the following section, we’ll dive into what is fueling the rise in the cost of healthcare.
Healthcare Costs Are Skyrocketing
It is known that healthcare costs have always been high, but we are currently at an all-time high and change is needed. According to the Centers for Medicare and Medicaid Services it is projected that spending in healthcare-related costs will increase 5.5 percent annually by 2027. Hospitals urgently need to make cost containment an area of focus.
Strata’s CEO Dan Michelson talks about the difficulty in sharing cost data with frontline decision makers in the healthcare system and how this influences the rising cost of care.
In the video, the Strata CEO shares the challenges most organizations face when trying to get cost information into the hands of their leaders and decision makers each day.
Data regarding the cost of care is not easily accessible for physicians working in hospitals, therefore driving up the cost of care. Although this is one of the biggest reasons for healthcare costs to rise, there are still other factors that influence the cost of care. There are various factors that drive the cost of care up including: Medical technological advances, aging population and labor costs. Below, you will read in more detail why these factors contribute to the rising cost of care.
Why Are We Seeing High Healthcare Costs?
- Medical Technological Advances: Technological advances are great in the medical industry because they improve life expectancy, tackle terminal illness and enable other medical improvements. Technological advances offer incredible support and improve the health of patients, but it is important to understand that the popular use of these expensive mix of services can lead to high healthcare expenses. While high costs for expensive tools and services may be out of our control, something we can control is how well these services are allocated. Knowing how to use these services effectively and efficiently will play a huge role in cost containment.
- Aging Population: The fastest-growing segment of the population is the 85-and-older age group. With an older population, the demand for healthcare rises, resulting in high healthcare costs. Considering v-based care allows hospitals to give proper care to patients while potentially saving money, as explained in a later section of this blog value-based care when caring for the elderly can help prevent illnesses and treat them in a  HYPERLINK “https://www.stratadecision.com/blog/top-5-episode-analytics-questions-answered/” bundle or episode based on their own needs. This strategy can potentially be used to reduce the cost of care for the elderly.
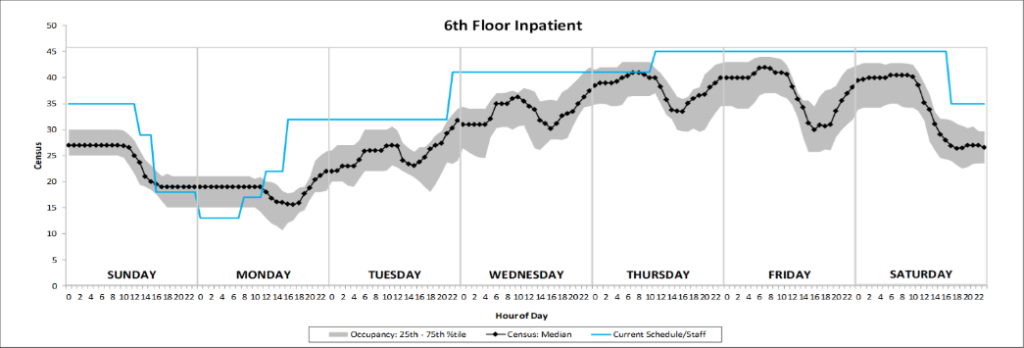
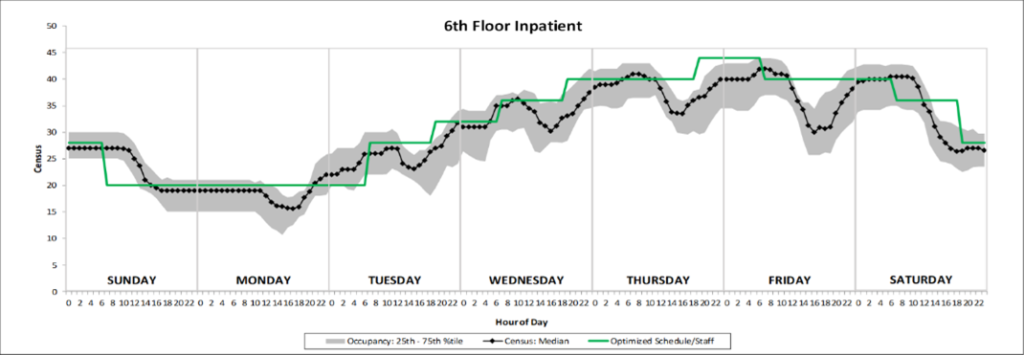
- Labor Costs: Labor Costs typically represent the largest category of healthcare expenses, for a number of reasons – but especially when schedules aren’t optimized. In an HFMA presentation on this topic, we shared a helpful graph on optimized staffing schedules. Refer to the two graphs presented side by side below. One graph shows how hospitals staff their workers and the gap between staffing and demand. Changing these staffing patterns can help with reducing significant waste. In the second graph, you can see what an optimized schedule would look like and the potential savings that can come out of it.
Cost Containment Trends
After analyzing a few hospitals, we’ve found there is a trend of strategies used by hospitals that benefit them by allowing them to cut down on costs. In the following section, you will learn of this group of strategies that can be implemented by your own hospital to lower your costs.
Telehealth: Transitioning towards telehealth benefits the patient experience and brings impactful saving measures to hospitals. Telehealth allows doctors and patients to have virtual visits where patients still get that one-on-one consultation, while saving both parties time. COVID-19 has restricted the capacity of hospitals, making it really challenging for patients to get prompt in-office visits. Telehealth can help ease this problem while helping hospitals save money. Patients can talk with their doctors through these telehealth visits without having to make unnecessary visits to the ER which can potentially cost thousands of dollars per visit.
A study done by researchers at the University of Queensland published by the Journal of Medical Research dives into all the benefits that come out of transitioning towards telehealth. The study results proclaim that telehealth realizes $361 per patient in savings, as well as reduces the number of hospitalizations.
Value Based Care: Value-based care is the idea of improving quality and outcomes for patients. Through value-based care, hospitals are looking to make healthcare proactive instead of reactive. The benefit of value-based care is that it allows hospitals to prevent problems before they occur which in the long term benefits hospitals by improving healthcare outcomes and reducing costs.
With the concept of value-based care, doctors and hospitals get paid based on outcomes, not on number of procedures, patients seen or how much they are charged. The benefit of this integrated system is that it allows us to create a plan coordinated specifically to the patients’ needs while working alongside a tailored team of doctors. It is important to know that value-based care is a long-term goal that prevents future complications, reduces hospitalizations and ER visits. The benefits of value-based care are that it produces better healthcare outcomes and lowers healthcare costs.
Data-Driven Strategies:
One of the most helpful strategies for cost containment is having accurate and useful information on the cost of care. Yale New Haven Health transitioned into using StrataJazz which in return helped them save $150 million. “One challenge for most healthcare providers is that they have little to no access to accurate, comprehensive and actionable information on the cost of care” stated Vincent Tammaro, executive vice president and CFO at Yale New Haven Health. Not having a system that helps you gain this accurate data makes it very challenging to make strategic and informed decisions. Luckily, there are vendors like Strata Decision Technology that can help hospitals with their financial planning.
Strata offers a platform of software and service solutions that help healthcare providers reduce the cost of care. StrataJazz® can help you fight the cost curve in healthcare by providing you with the correct advanced and integrated solutions. Learn more about specific strategies for creating a successful cost reduction plan in the next blog.